Aging
Frailty: What Families Need to Know About One of the Most Overlooked Risks to Senior Independence



In this article
Frailty is one of the strongest predictors of whether an older adult will remain independent, avoid falls, recover after illness, and continue living safely at home. Yet most families don’t recognize frailty until it has progressed into something serious: a fall, a hospitalization, or a sudden loss of mobility.
Frailty appears gradually, often through small physical and cognitive changes that families mistake for “just aging,” even though many adults remain strong and active into their nineties. Early recognition opens the door to slowing or even reversing decline.
What Is Frailty? A Simple Explanation
Frailty isn’t one condition, and it’s not just “getting older.” It’s a state where several systems in the body begin to weaken at the same time, making recovery from stress, illness, or injury much harder. In everyday terms, frailty is when someone’s strength, energy, and resilience start dropping together, making them more vulnerable to setbacks.
Common signs include walking more slowly, getting tired more easily, reduced activity, weaker grip strength, balance problems, or unintended weight loss. These changes don’t have to happen all at once. But when several appear together, they can signal that the body is losing some of its reserve.
What Frailty Looks Like in Everyday Life
Families usually notice frailty before a clinician formally diagnoses it. Day-to-day examples include holding onto furniture while walking, avoiding stairs, struggling with heavy doors or grocery bags, slowing down significantly, skipping meals, or losing interest in previously enjoyable routines. These are early functional changes that signal the body is beginning to struggle.
Frailty and Independence: Why It Matters So Much
Frailty reduces the body’s ability to recover from even mild health issues. As it progresses, everyday tasks become harder: cooking, bathing, cleaning, dressing, climbing stairs, or managing medications. A frail body is more prone to disability, falls, and hospitalization, and in many cases recovery becomes slow or incomplete.
Frailty can lead to loss of independence, difficulty performing activities of daily living (ADLs), and a higher likelihood of needing home support, rehabilitation, or long-term care. In its later stages, it may shorten life expectancy.
The Emotional Side: What Families Experience
Frailty can impose heavy emotional tolls on those affected and their families. Many caregivers describe fear, sadness, or frustration as they notice gradual changes. One geriatrician shared a story about her grandmother, who remained extremely active and independent into her 90s, shoveling snow, raking leaves, and living life fully until the last six months of her life, when frailty finally appeared. Families often ask whether frailty is simply “natural aging,” but examples like this show that decline is not always inevitable.
This emotional shift can be difficult for older adults too. They may feel embarrassed, frustrated, or fearful as they lose physical confidence. Families often struggle to balance helping with maintaining autonomy, one of the trickiest parts of caregiving.
Is Frailty Inevitable?
The short answer is no, frailty is not guaranteed with age. Many adults remain strong and functional throughout very old age. And even when frailty begins, it can often be managed, slowed, or partially reversed.
Protective factors that lower frailty risk include physical activity, good nutrition, stress management, social engagement, and proper management of chronic conditions. These habits act like “health deposits” that strengthen the body’s reserves over time.
Early Warning Signs Families Should Watch For
Frailty often begins with subtle functional changes. Some early indicators include:
Walking noticeably slower than usual
Reduced daily activity or fewer steps
Difficulty getting up from chairs or the bed
Trouble with stairs or uneven surfaces
Unintentional weight loss or reduced appetite
Fatigue or a general “slowing down”
Increasing fear of falling or avoiding movement
Unsteadiness or balance changes
These are all early markers of reduced functional reserve that often appear months or years before major declines.
Proactive Care: How to Manage Frailty
Health 3.0 focuses on catching decline early, not waiting for crises. Frailty shows why this matters. Once frailty leads to a fall or hospitalisation, recovery is much harder. Preventive care strengthens independence before issues escalate.
A proactive approach includes:
Staying physically active
Ensuring adequate protein and micronutrients
Managing chronic diseases and medications
Setting up the home to prevent falls
Keeping seniors socially and mentally engaged
Getting regular preventive checkups
Monitoring small day-to-day functional changes
These strategies overlap with the preventive recommendations for reducing frailty risk.
Health 3.0 reframes ageing by recognising that independence is preserved when small declines are noticed early, monitored consistently, and addressed before they escalate.
Why Staying Active Matters
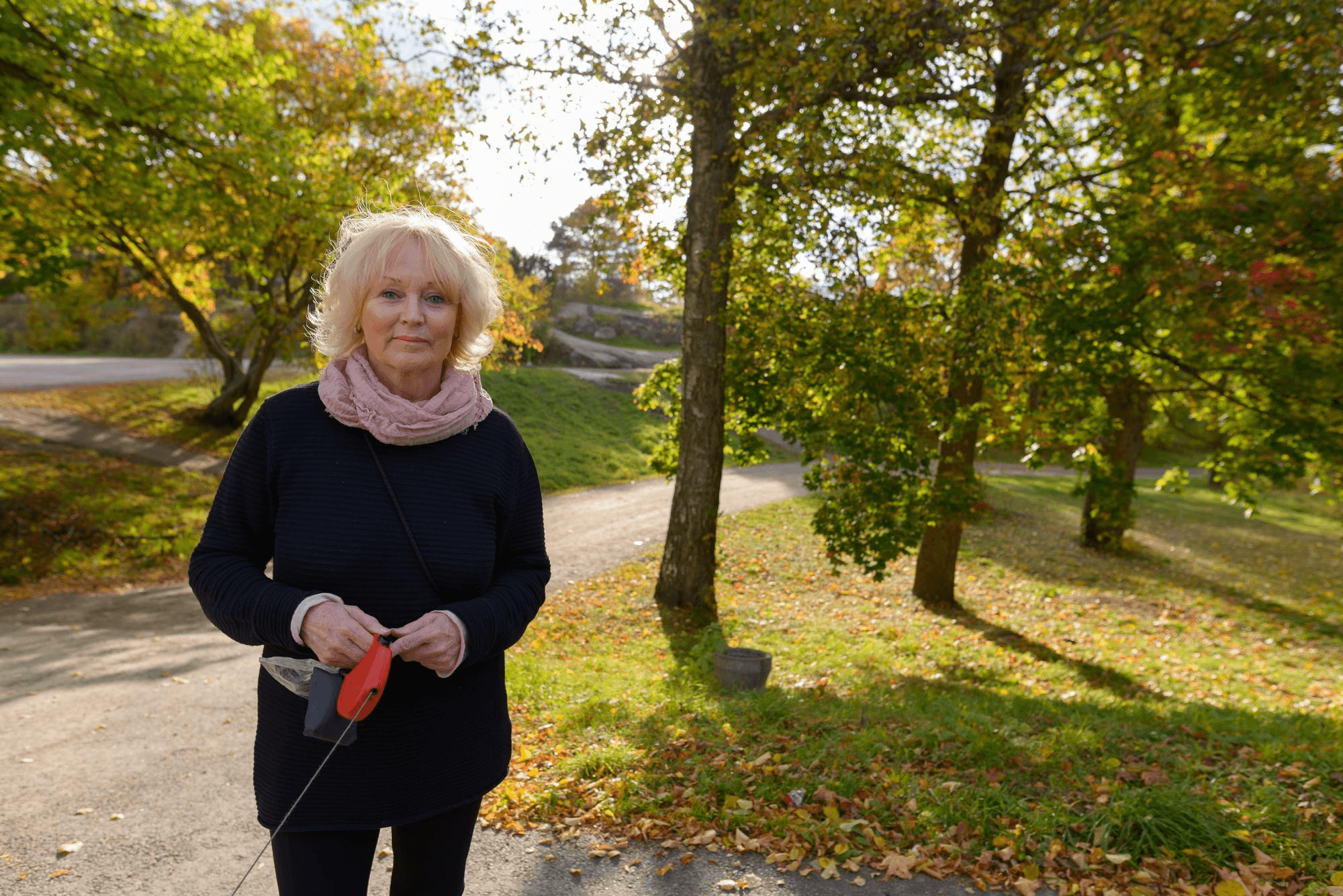
Physical activity is one of the strongest protectors against frailty. Even simple movement keeps muscles strong, improves balance, boosts energy, and helps the body recover from illness or injury. When seniors stop moving, decline happens faster.
The good news is that activity doesn’t have to be intense. A daily walk, light stretching, balance exercises, or simple strength training with bands or bodyweight can make everyday tasks like standing up, climbing stairs, and carrying groceries much easier and safer.
Strength training helps slow age-related muscle loss, while walking maintains endurance and joint mobility. The goal isn’t to push the body but to have consistent movement throughout the day.
Encouraging small, enjoyable activities can add years of strength and help older adults stay active on their own terms.
Why Frailty Awareness Matters
Frailty is one of the clearest predictors of future falls, hospitalisations, cognitive decline, and loss of independence. But it is also one of the most modifiable risks. Families who understand frailty and its early signs can intervene early and protect the health, dignity, and independence of the people they love.
Frailty doesn’t have to be a point of no return. With awareness, support, and preventive action, it can be a turning point toward strength rather than decline.
What HIA Is Doing
At HIA, we’re focused on catching frailty early, long before it leads to falls, hospitalization, or loss of independence.
We are:
• Unifying key risk indicators: gait speed, activity patterns, chronic conditions, medication load, and day-to-day functional changes into one clear framework for predicting decline.
• Setting quality standards for sensors: through our Silverline™ certification program, we are ensuring that the devices used to monitor older adults are accurate, reliable, and clinically meaningful.
• Turning complex clinical data into simple tools: families can use it to understand early warning signs and know when to take action.
Our mission is simple: help older adults stay stronger, safer, and independent for longer through proactive, prevention-first care.
Stay Connected with HIA
If your business is interested in working with the HIA on Dementia or Precision Cohort analysis of any kind, then contact us at partner@healthimpactalliance.com with a brief outline of your proposal.
Stay updated on the future of senior health technology; follow our LinkedIn and X for updates and insights. Interested in joining as a collaborator? Visit our website to learn more and get involved.
Sources:
Mayo Clinic Press, "Why Is Everyone Talking About Frailty?"
Cleveland Clinic, "Frailty"
Frailty is one of the strongest predictors of whether an older adult will remain independent, avoid falls, recover after illness, and continue living safely at home. Yet most families don’t recognize frailty until it has progressed into something serious: a fall, a hospitalization, or a sudden loss of mobility.
Frailty appears gradually, often through small physical and cognitive changes that families mistake for “just aging,” even though many adults remain strong and active into their nineties. Early recognition opens the door to slowing or even reversing decline.
What Is Frailty? A Simple Explanation
Frailty isn’t one condition, and it’s not just “getting older.” It’s a state where several systems in the body begin to weaken at the same time, making recovery from stress, illness, or injury much harder. In everyday terms, frailty is when someone’s strength, energy, and resilience start dropping together, making them more vulnerable to setbacks.
Common signs include walking more slowly, getting tired more easily, reduced activity, weaker grip strength, balance problems, or unintended weight loss. These changes don’t have to happen all at once. But when several appear together, they can signal that the body is losing some of its reserve.
What Frailty Looks Like in Everyday Life
Families usually notice frailty before a clinician formally diagnoses it. Day-to-day examples include holding onto furniture while walking, avoiding stairs, struggling with heavy doors or grocery bags, slowing down significantly, skipping meals, or losing interest in previously enjoyable routines. These are early functional changes that signal the body is beginning to struggle.
Frailty and Independence: Why It Matters So Much
Frailty reduces the body’s ability to recover from even mild health issues. As it progresses, everyday tasks become harder: cooking, bathing, cleaning, dressing, climbing stairs, or managing medications. A frail body is more prone to disability, falls, and hospitalization, and in many cases recovery becomes slow or incomplete.
Frailty can lead to loss of independence, difficulty performing activities of daily living (ADLs), and a higher likelihood of needing home support, rehabilitation, or long-term care. In its later stages, it may shorten life expectancy.
The Emotional Side: What Families Experience
Frailty can impose heavy emotional tolls on those affected and their families. Many caregivers describe fear, sadness, or frustration as they notice gradual changes. One geriatrician shared a story about her grandmother, who remained extremely active and independent into her 90s, shoveling snow, raking leaves, and living life fully until the last six months of her life, when frailty finally appeared. Families often ask whether frailty is simply “natural aging,” but examples like this show that decline is not always inevitable.
This emotional shift can be difficult for older adults too. They may feel embarrassed, frustrated, or fearful as they lose physical confidence. Families often struggle to balance helping with maintaining autonomy, one of the trickiest parts of caregiving.
Is Frailty Inevitable?
The short answer is no, frailty is not guaranteed with age. Many adults remain strong and functional throughout very old age. And even when frailty begins, it can often be managed, slowed, or partially reversed.
Protective factors that lower frailty risk include physical activity, good nutrition, stress management, social engagement, and proper management of chronic conditions. These habits act like “health deposits” that strengthen the body’s reserves over time.
Early Warning Signs Families Should Watch For
Frailty often begins with subtle functional changes. Some early indicators include:
Walking noticeably slower than usual
Reduced daily activity or fewer steps
Difficulty getting up from chairs or the bed
Trouble with stairs or uneven surfaces
Unintentional weight loss or reduced appetite
Fatigue or a general “slowing down”
Increasing fear of falling or avoiding movement
Unsteadiness or balance changes
These are all early markers of reduced functional reserve that often appear months or years before major declines.
Proactive Care: How to Manage Frailty
Health 3.0 focuses on catching decline early, not waiting for crises. Frailty shows why this matters. Once frailty leads to a fall or hospitalisation, recovery is much harder. Preventive care strengthens independence before issues escalate.
A proactive approach includes:
Staying physically active
Ensuring adequate protein and micronutrients
Managing chronic diseases and medications
Setting up the home to prevent falls
Keeping seniors socially and mentally engaged
Getting regular preventive checkups
Monitoring small day-to-day functional changes
These strategies overlap with the preventive recommendations for reducing frailty risk.
Health 3.0 reframes ageing by recognising that independence is preserved when small declines are noticed early, monitored consistently, and addressed before they escalate.
Why Staying Active Matters
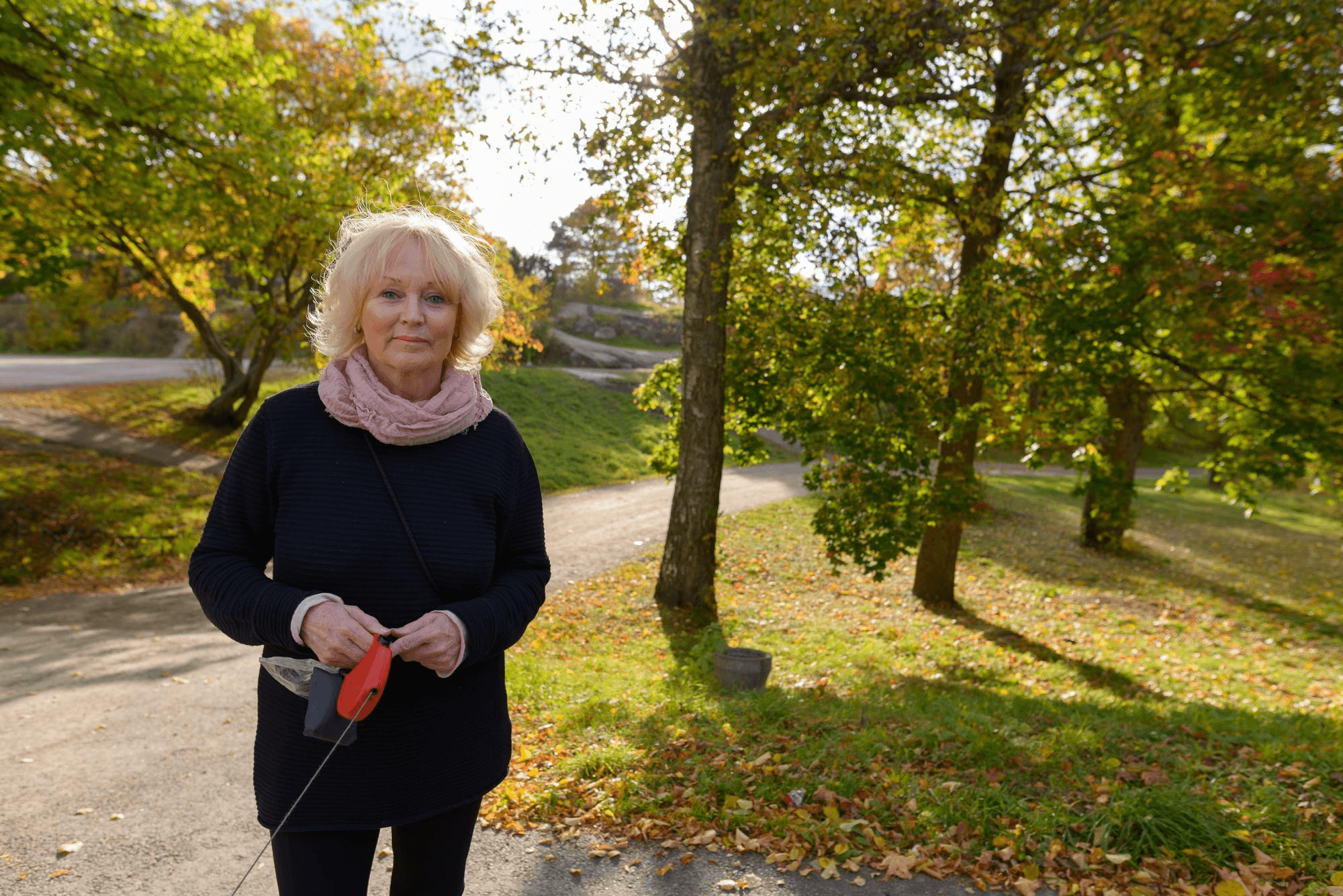
Physical activity is one of the strongest protectors against frailty. Even simple movement keeps muscles strong, improves balance, boosts energy, and helps the body recover from illness or injury. When seniors stop moving, decline happens faster.
The good news is that activity doesn’t have to be intense. A daily walk, light stretching, balance exercises, or simple strength training with bands or bodyweight can make everyday tasks like standing up, climbing stairs, and carrying groceries much easier and safer.
Strength training helps slow age-related muscle loss, while walking maintains endurance and joint mobility. The goal isn’t to push the body but to have consistent movement throughout the day.
Encouraging small, enjoyable activities can add years of strength and help older adults stay active on their own terms.
Why Frailty Awareness Matters
Frailty is one of the clearest predictors of future falls, hospitalisations, cognitive decline, and loss of independence. But it is also one of the most modifiable risks. Families who understand frailty and its early signs can intervene early and protect the health, dignity, and independence of the people they love.
Frailty doesn’t have to be a point of no return. With awareness, support, and preventive action, it can be a turning point toward strength rather than decline.
What HIA Is Doing
At HIA, we’re focused on catching frailty early, long before it leads to falls, hospitalization, or loss of independence.
We are:
• Unifying key risk indicators: gait speed, activity patterns, chronic conditions, medication load, and day-to-day functional changes into one clear framework for predicting decline.
• Setting quality standards for sensors: through our Silverline™ certification program, we are ensuring that the devices used to monitor older adults are accurate, reliable, and clinically meaningful.
• Turning complex clinical data into simple tools: families can use it to understand early warning signs and know when to take action.
Our mission is simple: help older adults stay stronger, safer, and independent for longer through proactive, prevention-first care.
Stay Connected with HIA
If your business is interested in working with the HIA on Dementia or Precision Cohort analysis of any kind, then contact us at partner@healthimpactalliance.com with a brief outline of your proposal.
Stay updated on the future of senior health technology; follow our LinkedIn and X for updates and insights. Interested in joining as a collaborator? Visit our website to learn more and get involved.
Sources:
Mayo Clinic Press, "Why Is Everyone Talking About Frailty?"
Cleveland Clinic, "Frailty"
Explore
U.S. Office
8 The Green, Suite B, Dover, DE, 19901, USA
London Office
London Office
London Office
167-169 Great Portland Street 5th Floor London, W1W 5PF, UK
167-169 Great Portland Street 5th Floor London, W1W 5PF, UK
167-169 Great Portland Street 5th Floor London, W1W 5PF, UK
167-169 Great Portland Street 5th Floor London, W1W 5PF, UK
167-169 Great Portland Street 5th Floor London, W1W 5PF, UK
Hong Kong Office
Unit 2406, 24/F, Low Block, Grand Millennium Plaza, 181 Queen's Road Central, Sheung Wan, Hong Kong
Stockholm Office
Brännkyrkagatan 76, 118 23 Stockholm Sweden
Shenzhen Office
Unit 2305, Building T1, Fangdacheng, No. 2 Longzhu 4th Road, Nanshan District, Shenzhen, People’s Republic of China